By Wendy Abdo, Craig Fowler, and Michael Broxterman of Pinnacle Health Group
A hospitals’ success is closely tied to the reputation of its medical staff. The ability to recruit, retain, and build physician loyalty is always a top concern. So, what are hospitals doing to stay on top? More and more we see them shifting toward physician employment.
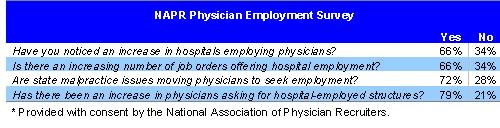
A recent survey conducted by the National Association of Physician Recruiters (NAPR), an association comprised of over 300 physician recruitment organizations, asked both in-house and independent physician recruiters about changes in physician employment. As shown in the table below, a majority of respondents saw an increase in the move toward employment for both hospitals and physicians.
Over the past year, many not-for-profit hospitals and health systems have revisited closer integration strategies with both new and existing physicians. Pinnacle Health Group, a leading recruitment firm, has noticed this trend firsthand through the type and structure of the physician searches it performs for its hospital clients.
Past Strategies
In the mid-1990’s, hospitals moved toward physician employment models in order to gain an advantage in managing utilization and controlling costs primarily because of managed care. The move, then, was to employ mostly primary care physicians rather than specialists and subspecialists. However, this movement was discontinued following the large losses suffered by hospitals.
During the 1990’s, physician recruitment was an offensive strategy used to build integrated delivery systems to deal with the advent of capitation. Yet, in most markets, capitation never materialized and hospitals were left with enormous infrastructure costs and losses at their employed physician subsidiaries.
Today’s Strategies
Hospital Influences
What are driving today’s hospitals back toward integration? There are three main factors:
- The need to take defensive measures to protect market share from surgery, imaging, and outpatient services as well as entrepreneurial physicians
- The desire to increase clinical services and reputation by recruiting “superstar” physicians
- Physician shortages, especially in less desirable geographic locations
Physician Influences
In the same way, physicians are also being influenced toward integration. Main drivers for them include:
- Difficult malpractice insurance environments and a lack of tort reform
- The need for stabilized and secure income through economic alignment
- The need for greater predictability of patient volume and the desire to improve patient care
Shared Influences
There are also drivers that both hospitals and physicians share in the move to integration as follows:
- The costly need of clinical information technology
- Consolidation among the larger payers that requires hospitals to build their leverage through physician loyalty, therefore, becoming indispensable to the payers
What’s Different Today?
The lessons learned in the mid-1990’s are a painful reminder of the financial pitfalls that can happen. That is why in today’s market the difference is in the approach. Hospitals today are more strategic-minded and prudent in developing their plans. They are also closely monitoring their results.
Today, there are fewer acquisitions than in the 1990’s. Instead, hospitals are moving toward less complex employment arrangements. The move toward physician employment can be seen through carefully constructed contracts that have clearly defined and agreed-upon productivity targets. Hospitals will employ primary care physicians, specialists, and subspecialists. In rural or less desirable markets, employment may be the only way to attract specialists who might not otherwise be convinced that there is a market to support them.
How Hospitals Benefit from Employment
Employing physicians enables hospitals to fund information technology needs at the physician’s office and keep them “connected” to the hospital. In addition, physician employment models oftentimes help hospitals keep from running into Stark issues such as purchasing and/or leasing of equipment for an independent physician.
Bringing a physician in on a guarantee can be risky. As hospitals extend their primary and secondary markets, it becomes more precarious for them to establish a physician. By hiring physicians, hospitals will lock up referrals. Setting up a physician under an employment model also gives the physician stability while the hospital’s goal of tying in referrals is realized.
While current trends show a definite increase in physician employment by hospitals, physician employment may not be for everyone. Local market dynamics as well as a hospital’s and physician’s long term strategies must be scrutinized closely before an employment plan is put into action.